
Editor’s Note: In honor of National Minority Health Month, we would like to shed some light on the issues of racial imbalance in cancer care.
In 2009, Jennifer Tseng, MD, and her team were scouring a National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End results (SEER) database when they noticed something surprising: Although black and white pancreatic cancer patients were recommended surgery at roughly the same rate, black patients were less likely to undergo the procedure.

Jennifer Tseng, MD
This research became the basis for a study in the journal Cancer, and it motivated Tseng’s team at the University of Massachusetts’ Surgical Outcomes Analysis & Research Program to continue exploring inequalities in cancer care.
“Racial disparities exist in medical and cancer care, and pancreatic cancer is no exception. We’re committed to eradicating these issues through our ongoing research,” said Tseng, who currently serves as chief of surgery at Boston Medical Center and a professor of surgery at Harvard Medical School as well as a 2006 Pancreatic Cancer Action Network (PanCAN) research grantee.
Cancer is projected to become the leading cause of death by 2020 in the United States. In 20 years, the American Society of Clinical Oncology estimates that 26.1 million Americans, all in need of continuing care, will be living with a history of cancer.
As the science and medical worlds continue to address key challenges in cancer care, a growing body of research is shining the light on a core issue: the role of race in the treatment of cancer.
Race as a Risk Factor
Figures from the United States 2018 census show that 76.6 percent of the U.S. population is white. Hispanic citizens compose 18.1 percent of the population, black citizens account for 13.4 percent, and Asian citizens make up 5.8 percent.
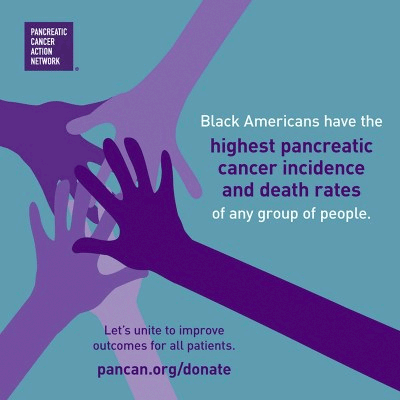
According to the NCI’s SEER data – the same database used in Tseng’s Cancer study – the pancreatic cancer incidence rate for black patients is up to 67 percent higher than other racial groups. The pancreatic cancer five-year survival rate is just 9 percent.
The rate of pancreatic cancer per 100,000 Americans is 10.0 for Asian patients, 11.2 for Hispanic patients, 12.6 for white patients and 15.5 for black patients. The death rate is 13.2, 10.9, 8.7 and 7.7 for black, white, Hispanic and Asian patients, respectively.
There is evidence that this disparity is more related to social/behavioral and access issues than biology.
Disparities in Cancer Treatment
Research shows that a significant proportion of pancreatic cancer patients remain undertreated, primarily due to nonclinical factors, including race, marital status and age. This undertreatment can surface in a number of ways.
Tseng’s team used SEER-Medicare data to compare treatments and outcomes between white and black pancreatic cancer patients.
 The researchers found for pancreatic cancer that had spread to regional lymph nodes and/or resectable (surgically removable) tissues, black patients were significantly less likely than white patients to have a consultation with a cancer specialist. Among patients who did have a consultation with an oncologist and/or surgeon, black patients were less likely to undergo chemotherapy or surgery.
The researchers found for pancreatic cancer that had spread to regional lymph nodes and/or resectable (surgically removable) tissues, black patients were significantly less likely than white patients to have a consultation with a cancer specialist. Among patients who did have a consultation with an oncologist and/or surgeon, black patients were less likely to undergo chemotherapy or surgery.
Similarly, a 2013 Annals of Surgical Oncology study found that although their resectability rates are generally comparable, treatment for black pancreatic cancer patients differed from current guidelines.
“In our SEER-Medicare study, our initial observation was that the lack of cancer-directed therapy, such as resection and adjuvant (post-surgery) therapy, could explain the difference in the survival rates between the two groups,” Tseng said.
Through their study of Massachusetts Department of Public Health data, Tseng’s team also found that black patients were less likely than white patients to travel more than 10 miles for pancreatic cancer surgery, which was associated with an increased likelihood of being treated at a low-volume center or community hospital.
For eligible patients, surgery is the best option for long-term survival of pancreatic cancer. Seeing pancreatic cancer specialists and physicians who diagnose and treat a high volume of pancreatic cancer patients improves outcomes.
PanCAN strongly recommends that patients consult with pancreatic cancer specialists who have experience diagnosing and treating the disease.
Clinical Trial Participation
Every treatment available today was approved through a clinical trial, and pancreatic cancer patients who participate in clinical research have better outcomes. Yet research shows that the patients who enroll in cancer clinical trials – the patients often receiving the most promising and leading-edge treatments – are overwhelmingly white.
In another study published in the journal Cancer, researchers at UC Davis Comprehensive Cancer Center found that less than 5 percent of clinical trial participants are non-white, and less than 2 percent of clinical cancer research focuses on non-white ethnic groups.
Although Congress established a mandate requiring the National Institutes of Health (NIH) trials to include enough minorities to determine whether they respond to treatment differently than other groups, only 6 percent of cancer trials were funded by the NIH in 2014. The remaining 94 percent were not subject to this regulation.
PanCAN maintains the most comprehensive, up-to-date database of pancreatic cancer clinical trials in the United States, which can be accessed with the free search tool, Clinical Trial Finder. PanCAN strongly recommends clinical trials at diagnosis and during every treatment decision.
Balancing the Scales of Cancer Care
With cancer diagnoses rising, research plays a crucial role in accelerating progress for cancer care – especially in pancreatic cancer, estimated to become the second leading cause of cancer-related death within the next few years.
PanCAN’s Patient Registry is a global online database designed to help researchers look for patterns in treatments, side effect management and diagnostics that will lead to improved treatment options and outcomes for patients. A key goal of the Patient Registry is to develop an accurate, representative database of those affected by pancreatic cancer.
Tseng is hopeful that research, like insights coming from the Patient Registry, will help spur new programs to combat racial discrepancies in care. In her role as the chair of surgery and surgeon-in-chief at Boston University and Boston Medical Center, her team has the opportunity to continue studying these disparities at a hospital with the largest share of minority and otherwise disadvantaged patients in New England.
Improving access to care is crucial to ending disparities, but it is a complex issue, she said. However, one factor that has been shown to improve outcomes in numerous disease populations, regardless of race, is adequate healthcare coverage. This is one key focus of her team’s research efforts.
“Our early findings suggest that disparities may be mitigated by an appropriate specialist’s referral and treatment,” Tseng said. “By identifying these barriers, we can help to define necessary intervention programs.”





