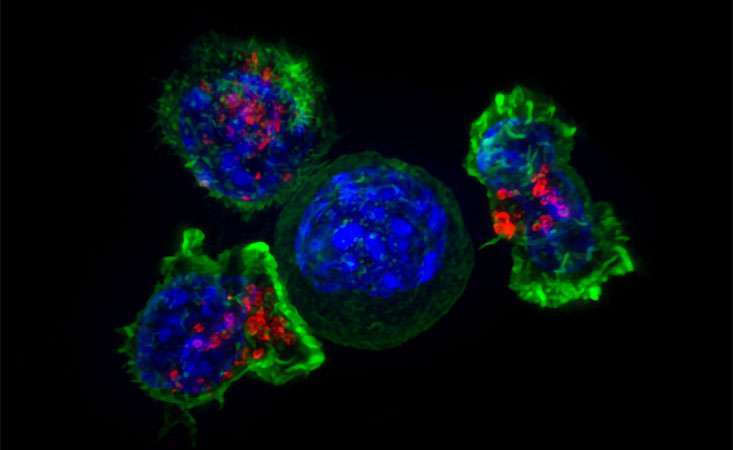
T-cells of the immune system (green and red) surround a cancer cell (blue). Credit: Alex Ritter, Jennifer Lippincott Schwartz and Gillian Griffiths, National Institutes of Health.
Editor’s note: We are republishing today’s blog in honor of Cancer Immunotherapy Month, which occurs each June.
Cancer immunotherapy involves empowering the patient’s immune system to recognize, attack and destroy cancer cells.
While remarkable results have been seen in some tumor types, like melanoma, the effectiveness of immunotherapy approaches in pancreatic cancer have been limited to date.
“A few critical steps are necessary for an immunotherapy approach to be successful,” explained Lynn Matrisian, PhD, MBA, chief science officer at the Pancreatic Cancer Action Network (PanCAN).
“First, the cells of the immune system need to recognize the cancer cells as ‘foreign,’ like they would recognize a virus or bacteria that invades the body. Next, cancer-fighting immune cells need to get close to the tumor and, finally, mechanisms that prevent the immune cells from working need to be eliminated or weakened.”
Pancreatic tumors are notoriously immunologically “cold,” which means the immune system needs extra boosts to stage an attack against the cancer cells.
Since cancer cells arise from healthy cells, it can be hard for the immune system to differentiate them. There are several immunotherapeutic strategies to overcome this challenge, including vaccines, which aim to spark immune recognition and response to the tumor. Another approach, called adoptive cell transfer, entails removing and re-injecting the patient with their own immune cells, specially trained to recognize the cancer cells.
In addition, drugs called checkpoint inhibitors aim to release the brakes on the immune system so that the tumor can’t protect itself from an immune attack. This approach has been proven successful in certain subsets of cancer patients, including pancreatic cancer, whose tumors have characteristics known as high microsatellite instability (MSI-high) or defective DNA mismatch repair (dMMR).
Tumors with MSI-high or dMMR characteristics have many, many more mutations than typical cancer cells.
“The immune system patrols the whole body, looking for pieces of proteins on the surface of cells that don’t match that person’s healthy cells,” Matrisian said. “When there are high numbers of mutated proteins on the surface of cancer cells, that gets the immune system’s attention.”
She continued, “So when tumors have MSI-high or dMMR characteristics, they should already be on the immune system’s radar. The final step is to ensure the tumor can’t hide itself from the immune system.”
A checkpoint inhibitor called Keytruda® was approved in May 2017 for the treatment of any solid tumor, anywhere in the body, with MSI-high or dMMR characteristics. This marked the first approval of a cancer drug based on the tumor’s molecular characteristics, instead of the tumor’s location in the body.
About 1 to 3 percent of pancreatic cancer patients have tumors that are MSI-high or dMMR. For these patients, like David Watson and Karen Kiernan, Keytruda has provided a new treatment option.
“Patients with pancreatic cancer can learn if their tumor has MSI-high or dMMR characteristics through PanCAN’s Know Your Tumor® precision medicine service,” Matrisian said. “In addition to these molecular alterations, other tumor changes can be found that align with certain types of targeted therapies or other treatment options.”
As for immunotherapy approaches for pancreatic cancer patients who do not qualify for Keytruda, researchers and clinicians are working to devise novel strategies to make immunotherapy more widely effective.
In the lab, PanCAN grantees and other scientists and working to understand how pancreatic cancer cells interact with cells of the immune system, and how to empower the immune cells to fend off the tumor. And, clinical trials are underway testing various immunotherapy approaches, alone and in combination with other types of treatment, in pancreatic cancer patients.
“We at PanCAN strongly recommend clinical trials at diagnosis and during every treatment decision,” Matrisian said, “and our Patient Services team can conduct a personalized clinical trials search for patients, caregivers and healthcare professionals.”
She added, “Whether or not immunotherapy is right for you or a loved one, it’s important to know about and consider all treatment options.”
Any treatments, including clinical trials, mentioned above may not be appropriate or available for all patients. Doctors take many things into account when prescribing treatments including the stage and type of cancer and the overall health of the patient. Contact PanCAN Patient Services for personalized treatment options.





