
The valuable skill of adapting to change, with as much care and understanding as possible, is particularly important for every patient and caregiver facing pancreatic cancer.
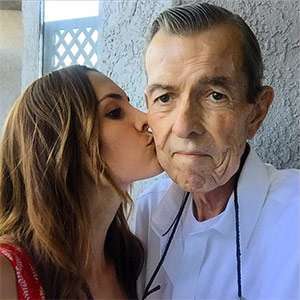
Lauren kissing her father, James, before he passed away in early 2017
Yoga and its counterpart meditation have for centuries been cultivating skillful adaptability for millions around the world, including Los Angeles-based Lauren Eckstrom. An eminent, nationally recognized yoga and meditation teacher, Eckstrom lost her father, James, to pancreatic cancer in early 2017. Her yoga and meditation practice not only prevented her from feeling like a victim to the disease but also empowered her to show up with more love and strength for her father and for herself.
When her dad was diagnosed, Eckstrom was practicing yoga 90 minutes to two hours for six days each week. But the shock of the pancreatic cancer diagnosis weighed so heavily on her heart and body that her yoga practice became much more gentle and slower.
As a caregiver, she confessed, “With all the appointments and the amount of information to process, I needed to slow down if I was going to have the energy to sustain what was coming up for us. It’s simply what my heart and body needed.”
Although Eckstrom’s yoga practice significantly transformed, her meditation discipline became more resolute. “Because the process of being with pancreatic cancer is so intense and involves so much, if you’re not in a place of getting in touch with who you really are, it’s very easy to be taken over by anger or frustration at the situation,” explained Eckstrom.
She found that meditation was central to her remaining present to the needs of her father and her stepmother, his primary caregiver. The contemplative technique enabled her to clearly see her core values and how she wanted to show up in this process, which was to be of compassionate service to them.
How is meditation and yoga good for patients and caregivers?
Many people have preconceived notions of what type of person does yoga or meditates – they look a certain way or they have a particular background. Eckstrom assures people: “Wherever you are in life and what’s happening with your body, there is a form of yoga and style of meditation that can be effective for you. There are specific approaches that work for various body types and levels of ability, which creates a space for everybody in these practices.”
The results of yoga and meditation are more qualitative than quantitative and take time, which is particularly critical for pancreatic cancer patients. Meditation develops a person’s ability to remain in the present, free of the anxieties of the past and future. Eckstrom adds that yoga offers a lot of potential value to patients and caregivers by taking a meditative practice and putting it into a beautiful form of movement, which can help process trauma differently and practice being present more easily.

A student receives a gentle adjustment from Lauren during yoga class (photo courtesy of Unplug Meditation)
“Time is so precious for pancreatic cancer patients and caregivers, and yoga and meditation can give them access points to spend time with greater quality,” Eckstrom said. “It’s critical for them to look at what they need right now based on their treatment program and their energy level. Then they can answer the question of what they want to most cultivate in their lives with this priceless time, such as their relationships.”
Eckstrom experienced this with her dad and stepmom. Her father wasn’t a religious man and didn’t practice traditional yoga or meditation. But he understood how good they felt doing these practices and how they were helping them.
“Because my stepmom and I valued our practices so much, we were able to support each other in that way. I would come over, and she would be able to have time on her own to do her practice, to be quiet with herself, fill her reserves back up and get back in touch with who she wanted to be in this journey with my dad and me.”
Eckstrom notes that if you have a particular faith or belief system, you get to bring them along into yoga and meditation. “As my father was moving through treatment, my stepmom took a meditation class at her Catholic church. They provided a welcoming space for both to belong.”
Aside from the personal value of the practices, the health benefits of yoga and meditation have been well researched by leading medical institutions and physicians including Jordan Berlin, MD, a Scientific & Medical Advisory Board member of the Pancreatic Cancer Action Network (PanCAN). He coauthored a study in 2016 on the potential therapeutic benefits of yoga during chemotherapy. Berlin commented, “I believe yoga and other mental activities that can improve flexibility, energy and/or a sense of well-being will be helpful in a person’s journey through their diagnosis of pancreatic cancer.”
Nicole Lise Feingold, Patient Services director for PanCAN, added, “Patients can regard complementary therapies such as yoga and meditation as a way to take some control over their health and improve their quality of life.”
What yoga and meditation practices are recommended for patients and caregivers?
Eckstrom suggests patients first speak with their healthcare team about doing restorative or gentle yoga practices, which should be taught by a Yoga Alliance certified teacher. She also offers this simple, even-balanced breath meditation to calm and center oneself:
- Inhale to the count of 4
- Pause to the count of 4
- Exhale to the count of 4
- Pause to the count of 2
- Repeat
- Do 5 rounds
For caregivers, she recommends that when they have time to do a practice to not get caught up in feeling like they need to accomplish something. It’s important for caregivers to listen to their bodies to determine if it would be more beneficial for them to get some rest with restorative yoga. Or maybe consider a more flowing class if they need to burn off anxious energy.
“When you see someone deteriorating whom you love, it puts you in close contact with your own mortality. Make use of that opportunity to take better care of your own body and mind with gratitude to be of better service to them. Hold the torch for them,” Eckstrom advised.
In terms of meditation, it’s helpful to realize that it can be difficult to sit with yourself when facing this disease or the loss of a loved one. It can seem easier to avoid it.

Lauren guiding a heart-centered meditation class (photo courtesy of Unplug Meditation)
“In meditation, it’s not going to be comfortable all the time, because meditation causes us to spend time with what’s true and what’s real for us,” cautioned Eckstrom. “And yet we can develop skills to be with what’s happening compassionately so that as we move through the treatment of a loved one we’re able to be with them 100 percent, to be a vessel and a vehicle of presence, and use our presence as medicine.”
In order to be with what’s uncomfortable, from sorrowful feelings to painful treatments, compassion is necessary to deal with it in a meaningful way, otherwise a person just suffers. Compassion enables people to connect with their own humanity and the humanity of others.
“Compassion is key to being in any positive relationship with our body, our mind, ourselves or each other,” Eckstrom said. “It doesn’t mean pretending everything’s okay. Compassion is ‘yes and…,’ which doesn’t always feel good. It’s saying, ‘Yes, I’m experiencing pain right now, but it won’t last,’ and that’s compassion – acknowledging what’s happening with that understanding.”
What is “mindfulness” and how can it benefit patients and caregivers?
With mindfulness, another common term for meditation, a patient or caregiver can pay attention to the moment precisely as it is and learn how to be with it, without running away or trying to fix it, which is a skill that can be very beneficial, especially moving through a pancreatic cancer experience.
Eckstrom points out that “when we try to hide our discomfort with TV or by wandering around online, we’re missing out on many moments of connection and healing.”
A patient or caregiver can develop a practice of mindfulness to deeply understand that everything is changing, physical sensations come and go, the breath rises and falls. Eckstrom said that “recognizing reality in this way can be of tremendous comfort during the toughest moments of the pancreatic cancer journey. To realize that a painful sensation or feeling will not last forever can help a patient or caregiver be with it without suffering nearly as much.”
A maxim that Eckstrom lived by throughout her journey with her father and the disease was a saying by renowned author and meditation teacher Ruth King: “Not perfect. Not permanent. Not personal.”
Eckstrom shared, “I was not perfect and neither was my father. Neither one of us is permanent. The pain and sickness was not permanent. The moments he expressed while in pain and confused were ultimately not about me. Recognizing all this made me value practically every moment we had together, including the hardest moments.”
Of the many definitions of yoga, one describes how the practice corrects the harmful turnings of the mind. This September, as the seasons turn outside in their natural, undisturbed way, consider how yoga can smooth out the turnings that occur within, no matter how troubling they may feel.
If you are thinking about beginning a yoga or meditation practice, it is important to consult with your doctor beforehand. For more information on pancreatic cancer and supportive resources, please contact PanCAN Patient Services.





